Isolation’s Immune Assault: How Loneliness Weakens Your Body’s Defenses
Social isolation and loneliness aren’t just emotional burdens—they’re biological threats that can compromise the immune system, leading to increased inflammation, reduced antiviral defenses, and heightened susceptibility to illnesses. Extensive research over the past decades has illuminated this connection, revealing that prolonged disconnection from others triggers a cascade of physiological changes akin to chronic stress. This report synthesizes key findings from scientific studies, highlighting mechanisms and evidence that underscore why fostering social bonds is crucial for health.
The Evidence from Landmark Studies
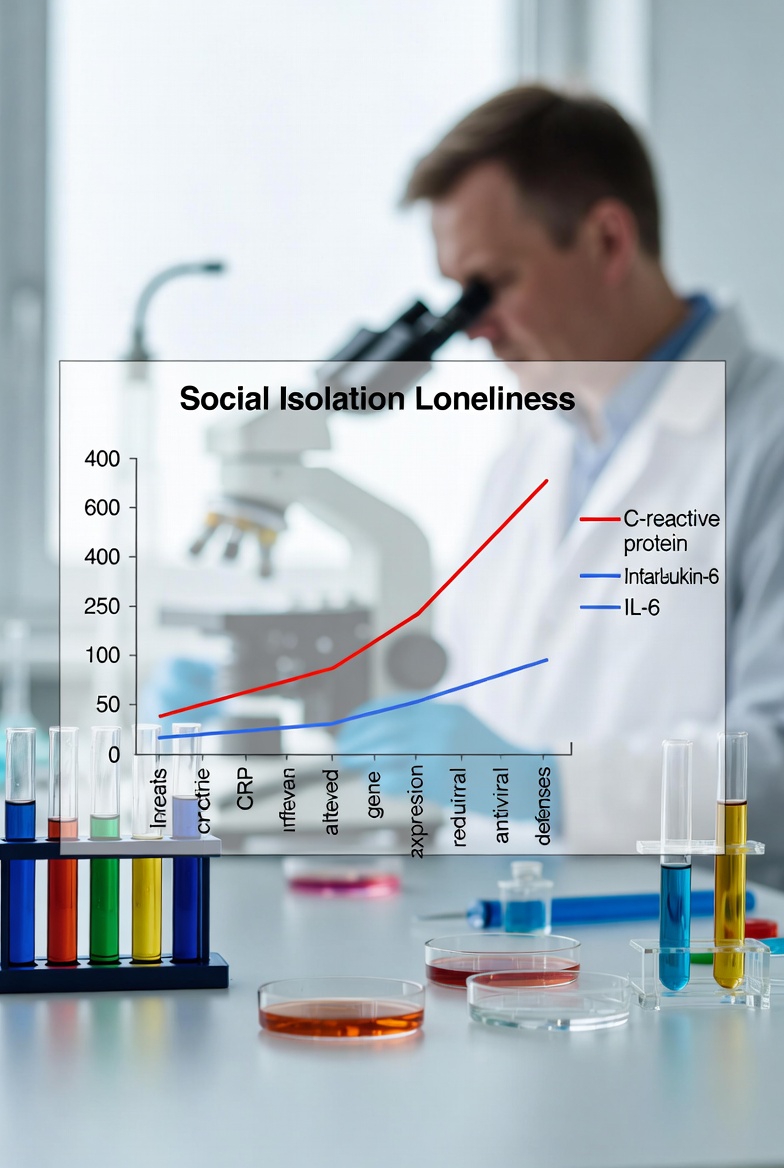
Numerous investigations have demonstrated a clear link between isolation and immune dysfunction. A multi-cohort analysis involving over 8,000 participants across Denmark, New Zealand, and the UK found that social isolation in childhood and adulthood is associated with elevated markers of systemic inflammation, such as soluble urokinase plasminogen activator receptor (suPAR), C-reactive protein (CRP), and interleukin-6 (IL-6). In medical patients, those living alone showed significantly higher suPAR levels, indicating chronic inflammation, while loneliness in mid-adulthood (but not early adulthood) correlated with increased suPAR.
In a comprehensive review framing loneliness as an “immunometabolic syndrome,” researchers detailed how it upregulates pro-inflammatory genes while downregulating antiviral ones through the conserved transcriptional response to adversity (CTRA). This pattern, observed in transcriptome analyses of leukocytes, leads to higher levels of cytokines like IL-6 and TNF-α, as well as acute-phase proteins such as CRP and fibrinogen. Studies across diverse populations, including older adults and breast cancer survivors, consistently show these elevations, linking loneliness to reduced immune cell proliferation, impaired antibody responses to vaccines, and increased oxidative stress.
A University of Chicago study further revealed cellular-level impacts: loneliness activates fight-or-flight signaling, boosting production of immature monocytes via norepinephrine, which heightens inflammation and impairs antiviral gene expression. In both humans and rhesus macaques, this resulted in a less effective immune response, with lonely individuals showing faster viral replication in infection models. The reciprocal nature—loneliness predicting future immune changes and vice versa—suggests a self-perpetuating cycle independent of factors like depression or social support.
Experimental evidence supports these observational findings. In a controlled study, lonely participants exposed to a mild bacterial endotoxin (Salmonella typhi) exhibited a four-fold increase in IL-6 levels compared to non-lonely counterparts, highlighting a dysregulated hyperimmune response. This aligns with broader reviews noting elevated pro-inflammatory markers like IL-1Ra and fibrinogen in lonely individuals, contributing to chronic low-grade inflammation and glucocorticoid desensitization.
The U.S. Surgeon General’s advisory on social connections emphasizes isolation’s role in infectious disease vulnerability. People with fewer social ties show weaker immune responses to viruses like the common cold and flu, with those having diverse social roles (e.g., six or more) exhibiting a four-fold lower risk of illness after exposure. Loneliness also correlates with diminished antibody responses to vaccines, including COVID-19, independent of prior exposure.
Underlying Mechanisms: Stress, Genes, and Inflammation
At the core of these effects are neuroendocrine pathways. Loneliness activates the hypothalamic-pituitary-adrenocortical (HPA) axis and sympathetic nervous system, leading to sustained cortisol release and glucocorticoid resistance. This desensitizes immune cells, allowing unchecked inflammation via pathways like NF-κB, while suppressing anti-inflammatory signals. Epigenetic changes, such as DNA methylation in immune genes, and genetic factors (e.g., BDNF polymorphisms) further exacerbate this.
Animal models reinforce human data: socially isolated primates and rodents display upregulated antimicrobial inflammation and downregulated antiviral defenses, mirroring human CTRA patterns. These alterations not only weaken defenses against infections but also contribute to broader health risks, including cardiovascular disease and premature mortality, with isolation’s impact rivaling smoking 15 cigarettes a day.
Implications and Future Directions
The cumulative evidence paints a stark picture: isolation isn’t benign; it reprograms the immune system toward inefficiency, increasing risks for infections, chronic diseases, and even faster disease progression (e.g., in HIV models). While short-term solitude may aid recovery, chronic loneliness demands intervention through social programs, therapy, or community building to mitigate these effects. Future research should explore interventions like mindfulness or digital connections to reverse immune dysregulation.
In summary, studies robustly confirm that isolation harms the immune system, urging a societal shift toward prioritizing connections for better health.
Citations
- Loneliness: An Immunometabolic Syndrome – PMC – https://pmc.ncbi.nlm.nih.gov/articles/PMC8618012
- Social isolation, loneliness, and inflammation: A multi-cohort investigation in early and mid-adulthood – https://www.sciencedirect.com/science/article/pii/S0889159123003562
- Does Loneliness Weaken the Immune System? – https://www.news-medical.net/health/Does-Loneliness-Weaken-the-Immune-System.aspx
- Our Epidemic of Loneliness and Isolation – HHS.gov – https://www.hhs.gov/sites/default/files/surgeon-general-social-connection-advisory.pdf
- Cardiovascular and immunological implications of social distancing in the context of COVID-19 – PMC – https://pmc.ncbi.nlm.nih.gov/articles/PMC7454335
- Loneliness triggers cellular changes that can cause illness, study shows – UChicago News – https://news.uchicago.edu/story/loneliness-triggers-cellular-changes-can-cause-illness-study-shows
- Social isolation, loneliness, and inflammation: A multi-cohort investigation in early and mid-adulthood – https://www.sciencedirect.com/science/article/pii/S0889159123003562
- Loneliness: An Immunometabolic Syndrome – PMC – https://pmc.ncbi.nlm.nih.gov/articles/PMC8618012
- Does Loneliness Weaken the Immune System? – https://www.news-medical.net/health/Does-Loneliness-Weaken-the-Immune-System.aspx
- Loneliness triggers cellular changes that can cause illness, study shows – UChicago News – https://news.uchicago.edu/story/loneliness-triggers-cellular-changes-can-cause-illness-study-shows
- Our Epidemic of Loneliness and Isolation – HHS.gov – https://www.hhs.gov/sites/default/files/surgeon-general-social-connection-advisory.pdf










Leave a Reply